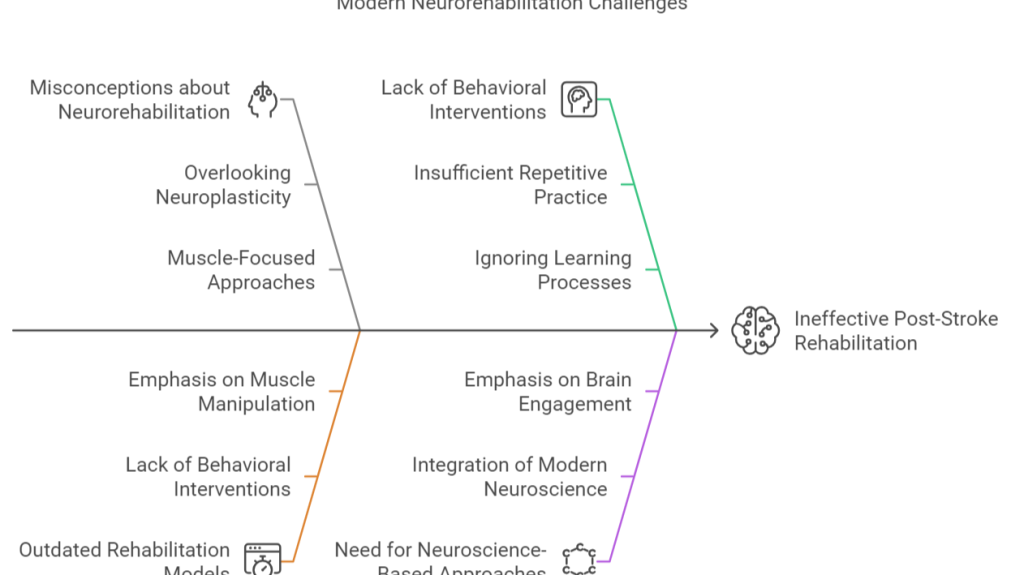
In light of the statement, «They won’t be able to help you in rehabilitation because your problem is in your brain,» we are forced to confront not just the profound misunderstanding embedded in such a remark, but also the deeper issue it reflects about the current state of clinical knowledge regarding neurorehabilitation. For those of us engaged in the domain of neurorehabilitation, this sentiment, though common, exposes a fundamental disconnect between the advancements in neuroscience and their translation into clinical practice. Beyond the initial reaction of dismay and frustration, we must ask ourselves: what are we, as professionals, failing to communicate about our field? How is it that the scope and efficacy of neurorehabilitation remain misunderstood, even by those working alongside us in the broader medical community?
The physician in this case was not entirely wrong in stating that the issue lies in the brain rather than the muscles. Indeed, following a stroke, the deficit is not at the level of the periphery; it is the brain’s capacity to initiate and control movement that is disrupted. Yet this statement, while correct in its assertion, reflects a residual framework inherited from 20th-century rehabilitation models—models which were primarily concerned with the musculoskeletal system and which, at best, acknowledged the nervous system only insofar as it was a static conductor of motor commands. In this view, muscles were seen as the weak links, the mechanical components needing repair or re-education, as though the CNS were but a passive observer, directing traffic rather than actively shaping movement.
This model persists in the clinic today. Many interventions still center around the muscle: passive stretching, manual facilitation, and manipulations by the therapist’s hands. The implicit assumption is that by ‘correcting’ the muscle, one somehow corrects the movement. However, this approach is not only inadequate—it is, at its core, misguided. It fails to account for the role of the central nervous system in generating movement and ignores the overwhelming evidence that movement control is a dynamic process, one that emerges from the interaction of brain, body, and environment. It is not the muscle that is the problem; the issue resides in how the brain engages with the body to execute skilled movement.
This is where the physician’s statement breaks down. The problem, indeed, is in the brain—but the conclusion that it is therefore beyond rehabilitation reflects a failure to appreciate the vast literature on neuroplasticity. Neuroscience in the 21st century, far from being reductionist, recognizes the capacity of the brain to reorganize after injury. Following a stroke, the brain does not simply lose its functions; it attempts to rewire. Neural circuits can adapt, and through targeted, repeated behavioral interventions, new patterns of activity can be established that compensate for the lost function. This phenomenon, known as neuroplasticity, is the basis for recovery.
Neuroplasticity, however, is not spontaneous. It does not emerge from passive manipulation of muscles or from the application of external forces. Neuroplasticity is fundamentally driven by behavior—by engaging the individual in the kinds of task-specific activities that stimulate the brain to forge new connections. Without behavioral intervention, the potential for plasticity remains dormant. This is why the outdated focus on muscles has proven ineffective. Rehabilitation must transition from the static, passive paradigms of orthopedics to the active, behavior-based models grounded in neuroscience.
A publication that illuminates this transition is Krakauer et al.’s «Neuroscience Needs Behavior: Correcting a Reductionist Bias.» In this work, the authors argue that too much of contemporary neuroscience is focused on understanding neural circuits in isolation, as though these circuits operate independently of the behaviors they support. This reductionist approach misses the core insight that neural circuits are not merely anatomical entities to be probed and manipulated, but are engaged in the production of specific behaviors. Understanding the brain, therefore, necessitates an equal emphasis on understanding behavior.
Neurorehabilitation must follow this path. Rather than focusing solely on the manipulation of muscles, we must shift our attention to how behavior shapes and is shaped by the brain. The recovery of movement, post-stroke or post-trauma, is not a matter of coaxing muscles into action; it is about re-educating the brain to engage with the body in meaningful ways. This requires a behavioral approach to neuroscience, where movement is understood not as a mechanical process but as a dynamic interaction between an organism and its environment.
To this end, we must emphasize that neurorehabilitation is a process of learning. Just as one learns to play a musical instrument or speak a new language, the brain relearns how to move following injury. This learning process is contingent on practice, feedback, and the adaptive capabilities of the nervous system. The central nervous system is not a static entity, but one that is capable of significant reorganization. Rehabilitation, therefore, is not about «fixing» muscles, but about reshaping the brain’s connections to those muscles through carefully designed, repetitive tasks that promote neuroplasticity.
This is where we, as neurorehabilitation specialists, must make our case. It is not enough to simply perform our interventions in the clinic; we must actively engage with other professionals, providing them with the evidence and frameworks they need to understand the principles of modern rehabilitation. We cannot assume that their training will fill in these gaps, nor can we expect them to automatically grasp the nuances of neuroplasticity. Instead, we must direct them to resources that elucidate the mechanisms of recovery.
I would recommend beginning with a foundational text such as Motor Learning (2019) by Krakauer et al., which provides a comprehensive overview of how the brain learns and relearns motor tasks. This paper not only details the process of motor learning from a neurobiological perspective but also connects this process to practical applications in rehabilitation. By understanding motor learning, one can begin to see that rehabilitation is not just possible for individuals with brain injuries—it is essential, because it taps into the very mechanisms by which the brain reorganizes itself.
In conclusion, the statement «your problem is in your brain» is true, but the assumption that this makes rehabilitation ineffective is not. The brain, through its capacity for plasticity, is capable of recovering function, but only if rehabilitation is approached in the right way. Neurorehabilitation must be informed by neuroscience, and neuroscience must be informed by behavior. Only by integrating these perspectives can we offer patients the best chance at recovery.
José López Sánchez
CEO @ Centro Europeo de Neurociencias | Intensive Therapy Specialist